Abstract
Background
The use of anti-PD-1 or PD-L1 inhibitors in combination with other anti-cancer agents was a priority for treating advanced non-small cell lung cancer (NSCLC) patients with considerable PD-L1 expression. However, studies seldom show the progression of liver metastases after using immune checkpoint inhibitors (ICIs).
Methods
Data were obtained from the Department of Pulmonary and Critical Care of Medicine, the First Affiliated Hospital of the Air Force Military Medical University. In the present study, we analyzed five non-small cell lung cancer (NSCLC) patients who had liver metastases after they were treated with pembrolizumab between 2019 and 2021. All of them had both stable primary lesions and liver progression with pembrolizumab intervention. Blood laboratory tests and imaging examinations were performed regularly during the treatment to assess the tumor responses of patients.
Results
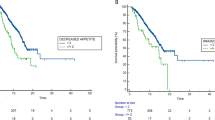
All patients displayed reduction or stability in the initial lesions as a result, but they also experienced the emergence of metastatic liver locations, which were regularly detected throughout immunotherapy. Additionally, the appearance of liver metastasis weakened their liver function gradually with the escalation of carcinoembryonic antigen, regarded as a predictor for evaluating the progression of tumors. These individuals were highly distinctive with hyper-progressive diseases associated with immunotherapy. We drew individualized intervention schemes for metastatic lesions in each patient and found that their life expectancy shared no significance given the restricting subjected population.
Conclusions
Our study indicated a clinical phenomenon after using immune checkpoint inhibitors and presented a necessity for implementing large scales clinical studies to manage NSCLC-oriented liver metastasis.




Similar content being viewed by others
Data availability
All data generated or analyzed in this study were oriented from a standardized clinical process and included in this published article.
Abbreviations
- ICIs:
-
Immune checkpoint inhibitor
- NSCLC:
-
Non-small cell lung cancer
- SCLC:
-
Small cell lung cancer
- PD-1:
-
Programmed cell death-1
- PD-L1:
-
Programmed cell death-ligand 1
- CT:
-
Computed tomography
- PET:
-
Positron emission tomography
- NGS:
-
Next-generation sequencing
- IHC:
-
Immunohistochemical
- PFS:
-
Progression-free survival
- OS:
-
Overall survival
- BLM:
-
Before liver metastasis
- LM:
-
Liver metastasis
- AFM:
-
After liver metastasis
- TACE:
-
Transhepatic arterial chemotherapy and embolization
- RFA:
-
Radiofrequency ablation
- SABR:
-
Stereotactic ablative radiotherapy
- WBRT:
-
Whole brain radiation therapy
References
Akinboro O, Larkins E, Pai-Scherf LH, Mathieu LN, Ren Y, Cheng J, Singh H (2022) FDA approval summary: pembrolizumab, atezolizumab, and cemiplimab-rwlc as single agents for first-line treatment of advanced/metastatic PD-L1-high NSCLC. Clin Cancer Res 28(11):2221–2228. https://doi.org/10.1158/1078-0432.Ccr-21-3844
Au L, Hatipoglu E, Robert de Massy M, Litchfield K, Beattie G, Rowan A, Turajlic S (2021) Determinants of anti-PD-1 response and resistance in clear cell renal cell carcinoma. Cancer Cell 39(11):1497-1518.e1411. https://doi.org/10.1016/j.ccell.2021.10.001
Balar AV, Kamat AM, Kulkarni GS, Uchio EM, Boormans JL, Roumiguié M, de Wit R (2021) Pembrolizumab monotherapy for the treatment of high-risk non-muscle-invasive bladder cancer unresponsive to BCG (KEYNOTE-057): an open-label, single-arm, multicentre, phase 2 study. Lancet Oncol 22(7):919–930. https://doi.org/10.1016/s1470-2045(21)00147-9
Bardia A, Hurvitz SA, Tolaney SM, Loirat D, Punie K, Oliveira M, Rugo HS (2021) Sacituzumab govitecan in metastatic triple-negative breast cancer. N Engl J Med 384(16):1529–1541. https://doi.org/10.1056/NEJMoa2028485
Botticelli A, Cirillo A, Scagnoli S, Cerbelli B, Strigari L, Cortellini, A., . . . Marchetti, P. (2020). The Agnostic Role of Site of Metastasis in Predicting Outcomes in Cancer Patients Treated with Immunotherapy. Vaccines (Basel), 8(2). doi:https://doi.org/10.3390/vaccines8020203
Chatterjee M, Turner DC, Felip E, Lena H, Cappuzzo F, Horn L, Fløtten Ø (2016) Systematic evaluation of pembrolizumab dosing in patients with advanced non-small-cell lung cancer. Ann Oncol 27(7):1291–1298. https://doi.org/10.1093/annonc/mdw174
Dolladille C, Ederhy S, Sassier M, Cautela J, Thuny F, Cohen AA, Alexandre J (2020) Immune checkpoint inhibitor rechallenge after immune-related adverse events in patients with cancer. JAMA Oncol 6(6):865–871. https://doi.org/10.1001/jamaoncol.2020.0726
Ettinger, D. S., Wood, D. E., Aisner, D. L., Akerley, W., Bauman, J., Chirieac, L. R., . . . Hughes, M. (2017). Non-Small Cell Lung Cancer, Version 5.2017, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw, 15(4), 504–535. https://doi.org/10.6004/jnccn.2017.0050
Gadgeel S, Rodríguez-Abreu D, Speranza G, Esteban E, Felip E, Dómine M, Garassino MC (2020a) Updated analysis from KEYNOTE-189: pembrolizumab or placebo plus pemetrexed and platinum for previously untreated metastatic nonsquamous non-small-cell lung cancer. J Clin Oncol 38(14):1505–1517. https://doi.org/10.1200/jco.19.03136
Gadgeel S, Rodríguez-Abreu D, Speranza G, Esteban E, Felip E, Dómine M, Garassino MC (2020b) Updated analysis from KEYNOTE-189: pembrolizumab or placebo plus pemetrexed and platinum for previously untreated metastatic nonsquamous non-small-cell lung cancer. J Clin Oncol 38(14):1505–1517. https://doi.org/10.1200/jco.19.03136
Grant MJ, Herbst RS, Goldberg SB (2021) Selecting the optimal immunotherapy regimen in driver-negative metastatic NSCLC. Nat Rev Clin Oncol 18(10):625–644. https://doi.org/10.1038/s41571-021-00520-1
Grunnet M, Sorensen JB (2012) Carcinoembryonic antigen (CEA) as tumor marker in lung cancer. Lung Cancer 76(2):138–143. https://doi.org/10.1016/j.lungcan.2011.11.012
Gubens, M. A., & Davies, M. (2019). NCCN Guidelines Updates: New Immunotherapy Strategies for Improving Outcomes in Non-Small Cell Lung Cancer. J Natl Compr Canc Netw, 17(5.5), 574–578. doi:https://doi.org/10.6004/jnccn.2019.5005
Guo, X., Shao, J., Zhai, B., Zou, Q., Yan, J., Gu, H., & Wang, G. (2020). Relationship and prognostic significance between preoperative serum albumin to globulin ratio and CT features of non-small cell lung cancer. Eur J Radiol, 128, 109039. doi:https://doi.org/10.1016/j.ejrad.2020.109039
Juarez-Garcia A, Sharma R, Hunger M, Kayaniyil S, Penrod JR, Chouaïd C (2022) Real-world effectiveness of immunotherapies in pre-treated, advanced non-small cell lung cancer patients: a systematic literature review. Lung Cancer 166:205–220. https://doi.org/10.1016/j.lungcan.2022.03.008
Kim CG, Kim C, Yoon SE, Kim KH, Choi SJ, Kang B, Lim HY (2021a) Hyperprogressive disease during PD-1 blockade in patients with advanced hepatocellular carcinoma. J Hepatol 74(2):350–359. https://doi.org/10.1016/j.jhep.2020.08.010
Kim S, Kim SA, Nam GH, Hong Y, Kim GB, Choi Y, Kim IS (2021b). In situ immunogenic clearance induced by a combination of photodynamic therapy and rho-kinase inhibition sensitizes immune checkpoint blockade response to elicit systemic antitumor immunity against intraocular melanoma and its metastasis. J Immunother Cancer, 9(1). https://doi.org/10.1136/jitc-2020-001481
Lai J, Beavis PA, Li J, Darcy PK (2021) Augmenting adoptive T-cell immunotherapy by targeting the PD-1/PD-L1 Axis. Cancer Res 81(23):5803–5805. https://doi.org/10.1158/0008-5472.Can-21-3548
Langer CJ, Gadgeel SM, Borghaei H, Papadimitrakopoulou VA, Patnaik A, Powell SF, Gandhi L (2016) Carboplatin and pemetrexed with or without pembrolizumab for advanced, non-squamous non-small-cell lung cancer: a randomised, phase 2 cohort of the open-label KEYNOTE-021 study. Lancet Oncol 17(11):1497–1508. https://doi.org/10.1016/s1470-2045(16)30498-3
Li X, Ramadori P, Pfister D, Seehawer M, Zender L, Heikenwalder M (2021) The immunological and metabolic landscape in primary and metastatic liver cancer. Nat Rev Cancer 21(9):541–557. https://doi.org/10.1038/s41568-021-00383-9
Medina PJ, Adams VR (2016) PD-1 pathway inhibitors: immuno-oncology agents for restoring antitumor immune responses. Pharmacotherapy 36(3):317–334. https://doi.org/10.1002/phar.1714
Mok TSK, Wu YL, Kudaba I, Kowalski DM, Cho BC, Turna HZ, Lopes G (2019) Pembrolizumab versus chemotherapy for previously untreated, PD-L1-expressing, locally advanced or metastatic non-small-cell lung cancer (KEYNOTE-042): a randomised, open-label, controlled, phase 3 trial. Lancet 393(10183):1819–1830. https://doi.org/10.1016/s0140-6736(18)32409-7
Osorio JC, Arbour KC, Le DT, Durham JN, Plodkowski AJ, Halpenny DF, Hellmann MD (2019) Lesion-level response dynamics to programmed cell death protein (PD-1) Blockade. J Clin Oncol 37(36):3546–3555. https://doi.org/10.1200/jco.19.00709
Planchard D, Popat S, Kerr K, Novello S, Smit EF, Faivre-Finn C, Peters S (2018) Metastatic non-small cell lung cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol, 29 Suppl 4, iv192-iv237. doi:https://doi.org/10.1093/annonc/mdy275
Powell SF, Rodríguez-Abreu D, Langer CJ, Tafreshi A, Paz-Ares L, Kopp HG, Garassino MC (2021) Outcomes with pembrolizumab plus platinum-based chemotherapy for patients with NSCLC and stable brain metastases: pooled analysis of KEYNOTE-021, -189, and -407. J Thorac Oncol 16(11):1883–1892. https://doi.org/10.1016/j.jtho.2021.06.020
Reck M, Rodríguez-Abreu D, Robinson AG, Hui R, Csőszi T, Fülöp A, Brahmer JR (2021) Five-year outcomes with pembrolizumab versus chemotherapy for metastatic non-small-cell lung cancer with PD-L1 tumor proportion score ≥ 50. J Clin Oncol 39(21):2339–2349. https://doi.org/10.1200/jco.21.00174
Robert C, Schachter J, Long GV, Arance A, Grob JJ, Mortier L, Ribas A (2015) Pembrolizumab versus ipilimumab in advanced melanoma. N Engl J Med 372(26):2521–2532. https://doi.org/10.1056/NEJMoa1503093
Schizas D, Charalampakis N, Kole C, Economopoulou P, Koustas E, Gkotsis E, Karamouzis MV (2020) Immunotherapy for pancreatic cancer: A 2020 update. Cancer Treat Rev, 86: 102016. doi:https://doi.org/10.1016/j.ctrv.2020.102016
Topalian SL, Hodi FS, Brahmer JR, Gettinger SN, Smith DC, McDermott DF, Sznol M (2012) Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med 366(26):2443–2454. https://doi.org/10.1056/NEJMoa1200690
Tumeh PC, Hellmann MD, Hamid O, Tsai KK, Loo KL, Gubens MA, Daud A (2017) Liver metastasis and treatment outcome with anti-PD-1 monoclonal antibody in patients with melanoma and NSCLC. Cancer Immunol Res 5(5):417–424. https://doi.org/10.1158/2326-6066.Cir-16-0325
Wang X, Ji Q, Yan X, Lian B, Si L, Chi Z, Guo J (2020) The impact of liver metastasis on anti-PD-1 monoclonal antibody monotherapy in advanced melanoma: analysis of five clinical studies. Front Oncol, 10:546604. https://doi.org/10.3389/fonc.2020.546604
Wood SL, Pernemalm M, Crosbie PA, Whetton AD (2014) The role of the tumor-microenvironment in lung cancer-metastasis and its relationship to potential therapeutic targets. Cancer Treat Rev 40(4):558–566. https://doi.org/10.1016/j.ctrv.2013.10.001
Wu YL, Zhang L, Fan Y, Zhou J, Zhang L, Zhou Q, Mok T (2021) Randomized clinical trial of pembrolizumab vs chemotherapy for previously untreated Chinese patients with PD-L1-positive locally advanced or metastatic non-small-cell lung cancer: KEYNOTE-042 China Study. Int J Cancer 148(9):2313–2320. https://doi.org/10.1002/ijc.33399
Yu J, Green MD, Li S, Sun Y, Journey SN, Choi J E, Zou W (2021). Liver metastasis restrains immunotherapy efficacy via macrophage-mediated T cell elimination. Nat Med, 27(1), 152-164. doi:https://doi.org/10.1038/s41591-020-1131-x
Zhang Y, Huang S, Gong D, Qin Y, Shen Q (2010) Programmed death-1 upregulation is correlated with dysfunction of tumor-infiltrating CD8+ T lymphocytes in human non-small cell lung cancer. Cell Mol Immunol 7(5):389–395. https://doi.org/10.1038/cmi.2010.28
Zhou C, Wang J, Wang B, Cheng Y, Wang Z, Han B, Qin S (2021) Chinese experts consensus on immune checkpoint inhibitors for non-small cell lung cancer (2020 Version). Zhongguo Fei Ai Za Zhi 24(4):217–235. https://doi.org/10.3779/j.issn.1009-3419.2021.101.13
Zielinski C, Knapp S, Mascaux C, Hirsch F (2013) Rationale for targeting the immune system through checkpoint molecule blockade in the treatment of non-small-cell lung cancer. Ann Oncol 24(5):1170–1179. https://doi.org/10.1093/annonc/mds647
Acknowledgements
The authors thank Pro. Lu Wang for her assistance in evaluating pathological diagnosis. We also thank Pro. Hong Yin and Pro. Xue Gong for their altruistic help in sharing knowledge in imaging and ultrasound.
Funding
This study was funded by grants from the Booster project of the Air Force Military Medical University (#2021LC2115) and the National Natural Science Foundation of China (#81902316).
Author information
Authors and Affiliations
Contributions
DQ and HX collected the relative information from patients and analyzed these data; MW was responsible for the calibration of the data and its follow-up; PJ, NC, XY, and YZ presented the indicated cases with original data; ZR was responsible for statistical analysis; XC helped to diagnose liver metastasis with professional assistance. YZ described the typesetting and wrote the manuscript; JZ presented the concept and design. All authors had read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors have not disclosed any competing interests.
Ethics approval and consent to participate
This study was approved by the Ethics Committee of the First Affiliated Hospital of the Air Force Medical University. Clinical cases included in this paper have signed informed consent based on the voluntary principle.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Qiu, D., Xi, H., Wang, M. et al. The debatable role of immune checkpoint blockade therapy in lung adenocarcinoma-oriented liver metastatic malignant lesions. J Cancer Res Clin Oncol 149, 5791–5802 (2023). https://doi.org/10.1007/s00432-022-04538-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-022-04538-5